 Even though different people respond to stents in different ways, I suspect anyone who’s ever lived with a ureteral stent remembers the experience. I have had two, and both were, indeed, memorable.
Even though different people respond to stents in different ways, I suspect anyone who’s ever lived with a ureteral stent remembers the experience. I have had two, and both were, indeed, memorable.
Prior to undergoing a pyeloplasty, (a surgical procedure to correct a urinary tract obstruction) I was informed that a stent would be in place for about seven weeks. I also recall being told, or perhaps reading, that such stents cause “discomfort” in some patients. In my mind the term “discomfort” equates to nothing more than an annoyance or a nuisance, so going into the surgery I was not overly concerned. For the first couple of days following surgery, perhaps because of post-surgical pain killers, it seemed the stent would be absolutely no problem. I could hardly feel it. “This will be a piece of cake,” I thought.
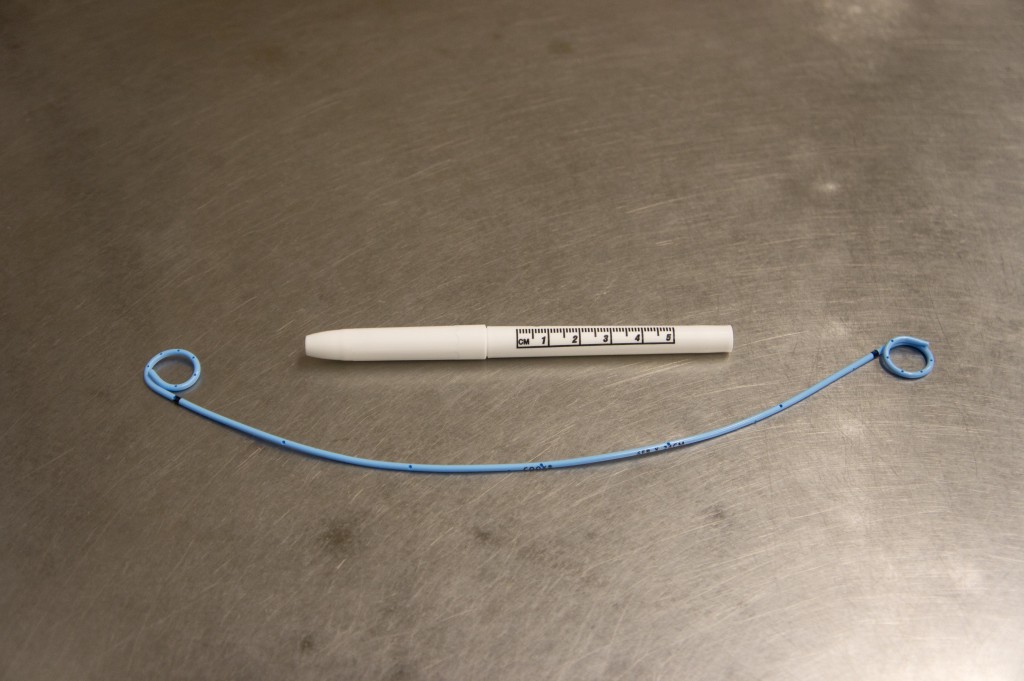
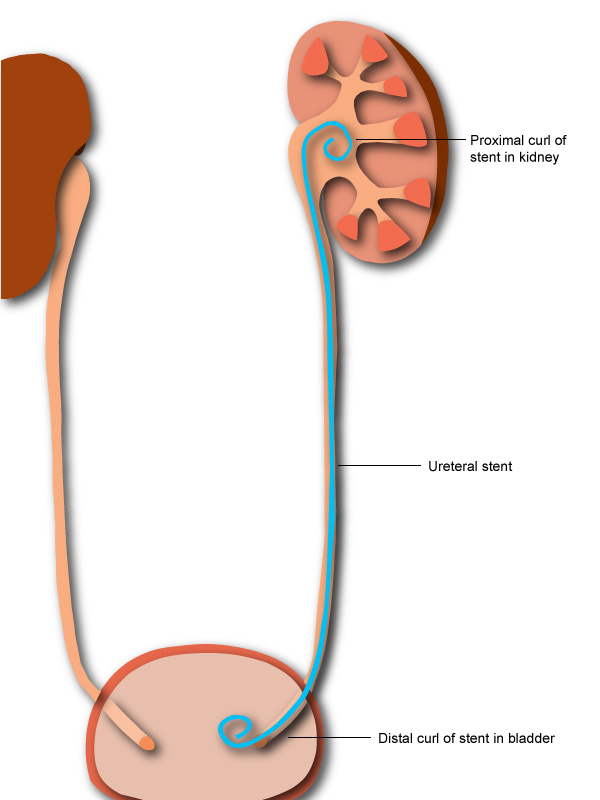
Then, shortly after going home, I became increasingly aware that some apparently sharp object was attempting to drill a hole through the wall of my bladder. In fact, the image of a shish-kabob skewer came to mind. At the same time, there was the sensation that something was tugging on my right kidney, trying to pull it down from its usual location. It was difficult to find comfortable positions…and it felt as though gravity was becoming my worst enemy. Urination was frequent and painful, and my urine continued to be bloody for the entire seven weeks. Involuntary tears came to my eyes and waves of nausea were common. Finally, I discovered that sitting in a recliner and tipping it back approximately half way seemed to relieve the worst of the pain, and that allowed me to get a little sleep at night.
After seven long weeks, I welcomed the removal of that first stent. A generous application of lidocaine made the procedure entirely tolerable, and I watched on the monitor as the stent was grabbed and the upper curly-cue began its descent down through the ureter. Once I was free of the stent, the relief I felt far surpassed the minor discomfort associated with its removal.
About a month later, I accepted a second stent with guarded optimism. This one was placed following lithotripsy for a 1+ cm stone in my left kidney. It seemed logical to me, since this ureter was not compromised or swollen, that this stent should not hurt nearly as much as the first. Unfortunately, I was wrong about that. Once again, the same familiar painful and distressing physical sensations returned. And once again I sought relief in the recliner. The stent allowed stone fragments to pass, but I was elated to be rid of it after only three weeks.
 The second stent experience left me with a new determination to do everything I could to prevent future stone formation. If making a few adjustments, such as drinking much more water each day, can prevent new stones and another stent placement sometime down the road, then I was ready to change old habits. Accepting the inevitability of new stones, then treating them as they become problematic, is no longer acceptable. My new plan is to be well-informed and pro-active and do all I can to discourage new stone formation. In fact, it’s the vivid memory of previous painful stents that continues to be the most powerful motivator. In a way, then, those stents are still serving a most valuable purpose, and I should remain grateful for them.
The second stent experience left me with a new determination to do everything I could to prevent future stone formation. If making a few adjustments, such as drinking much more water each day, can prevent new stones and another stent placement sometime down the road, then I was ready to change old habits. Accepting the inevitability of new stones, then treating them as they become problematic, is no longer acceptable. My new plan is to be well-informed and pro-active and do all I can to discourage new stone formation. In fact, it’s the vivid memory of previous painful stents that continues to be the most powerful motivator. In a way, then, those stents are still serving a most valuable purpose, and I should remain grateful for them.
Editors note: Bonnie writes about her experiences as a stone patient in her posts. If you have experiences as a patient you would like to share, feel free to add a comment or send her an email at: ask@kidneystoners.org
Going through the same thing right now. “Discomfort” is right. So much worse than passing a kidney stone. It’s a constant nagging relentless extreme discomfort. I won’t call it pain because I can tolerate a lot of pain, but this is making me insane. It’s like the most irritation any part of my body has ever felt. I hate that little tube, I hate it to hell. Now pain, that comes when urinating, holy hell. There are two things in my life that have caused enough pain to make me vomit, a kidney stone, and a stent. When peeing hurts so much that it makes you throw up, I don’t care who you are that has a mental effect. If you ever want to be terrified of going to the bathroom every time get a stent. Then they want you to drink lots and lots of fluids, and you do so fully knowing that every sip is another second of immense pain in the future.
I’ve had my uteral stents in 3 months the worst 2 things about it is peeing constantly and the burning after peeing. I am tired all the time I have 10 days to go. Am not afraid to get this terrible thing out
Has anyone ever had their kidney blasted with sound waves but not put a stent in after? I have passed kidney stones with way less discomfort and pain than the stent caused me.
So after googling “why do bilateral stents hurt so bad” I found this post. I thought I was over-reacting about the pain of these two stents, and I have a high pain tolerance. Never had a kidney stone but when I was at a prenatal appointment in Oct my doc said I had high levels of white blood cells, but kidneys came back fine. She said she was prescribing antibiotics just in case, as I had severe sepsis two pregnancies ago and was in ICU and almost died. Anyway. Went to doc again in mid Nov with what i thought was a kidney infection. Admitted to hospital and after 4 days they finally saw that it was an 8mm kidney stone. I am 9 months pregnant. When they put stent in left kidney and my bladder they saw my right kidney is very enlarged(more than what is normal in pregnancy)and had blockage so they put a stent in that kidney also. Woke up from surgery with horrible cramping, horrible pain. Can feel the stents, horrible pain when urinating. Oftentimes it hurts to even stand up straight. Add in an 8lb+ baby sitting on my bladder😬. Every time baby moves its shooting pain. Its been over a week and I hoped the pain and irritation would have subsided. It hasn’t. When I deliver baby they will do a CATscan to see exactly whats going on and make a plan then. All they could really do is prescribe antibiotics until i deliver and do the stents, all options are off the table since I am pregnant(and I’m not doing a tube out of my back with a bag to catch urine.)
Urologist was honest and said some people have no issues with stents, others have “mild pain” and others are in pain. Seems like 90% of people are in pain though. I am hoping the stents can be removed asap, this is miserable. I feel like all I can do is the bare minimum and then sit in an armchair.
I don’t have stones however a long history of chronic pain caused by hydronephrosis and megaureter. I had my first stent inserted 2 weeks ago while my doctor decides what to do next. I was dreading the stent and was filled with anxiety. It hasn’t been as bad as I imagined.
As soon as I woke from the procedure I drank loads of water. Peeing for the first few days was very painful however I tried to breathe through it and continued to have loads of water and ural a few times a day. My dr also has me on antibiotics for the duration of the stent.
I am extremely fatigued however I am fortunate I am able to rest. My sleep is interrupted by needing to get up every few hours each night. I have had a couple of nights of pain keeping me up and in tears however a wheat pack helped and the next day I started having ural again plus increasing my water intake. It helps.
I also wonder if pain and discomfort increase after having bigger meals and red meat.
Does anyone have good news stories following pyeloplasty?
Hi all, I’ve been “suffering” with 2 JJs since the end of May/2020, specially during urination (pain in the flanks), but last month I started taking Solofenacin Succinate 5mg before going to bed and it really made a difference. I am also taking tamsulosin 400mg by the morning. Now that pain during the end of the urination has mostly gone. I advise speaking to your GP about Solofenacin. Just wanted to share my experience and maybe help someone else that is currently suffering this terrible pain.
I have lived with Uretural stent in my right kidney since 2012. I have had to get the stent replaced every 3 months. I had too many laparoscopic surgeries performed on my large and small intestines because of acute Ulcerative Colitis. I have no life because of it. All I do is work at The Home Depot, all the while, wishing I had a pain pill or two. The Urologist refuses to prescribe oxycodone for the torture that I endure. Constant sharp kidney and bladder pain with Nephritis and kidney stones. It feels like I have a length of rusty barbed wire in my side. It twitches and throbs daily. This cursed condition causes me to be passively suicidal, I don’t know what I can do to fix this living nightmare. People at work think that I have an anger management issue. They have no idea what it’s like to exist in constant pain, its mentally and physically exhausting. Please help me..anyone.
I had a stent following lithotripsy. It was only in 6 days and came out easily. But the profound pain that followed has been as bad as the kidney stone pain. I am down to 3 Percocet and I’m terrified my doc won’t renew it. It’s been only 3 days since the stent removal and I am unable to function. I can’t imagine going much longer.
Joseph – I am so sorry to hear that you are in chronic pain. I’ve been in pain for only 7 days, ever since my stent was put in, and it’s been dreadful. I can’t imagine experiencing this long term. Can you talk to a counselor who specializes in chronic pain? I really think you should talk to a professional.
Joseph, You are most certainly in my prayers having to deal with such a horrible condition. I have had my stent for about 4 weeks now, have lost 15 pounds due to the constant nausea it has caused me. My saving grace is I have a desk job where I can sit with the heating pad wrapped around me—the ONLY thing that has provided me any relief. My urologist is proposing a second round of lithotripsy for the stone that has caused the need for this stent instead of urteroscopy—I called his office yesterday to ask why but he was not in. I left a message to request that he reconsider due to not only my sanity but that of my husband who is being forced to pick up my slack. The lithotripsy didn’t even MOVE the stone much less break it up so WHY do it again?!?! I don’t understand why doctors want to TORTURE patients like they do. The definition of insanity is doing the same thing over and over and expecting a different result…. I HAVE tried to move to a different dr. BUT since I had a device implanted by one, another won’t touch me. Isn’t that grand?
I pray by now you have found a caring doctor to help you live your life in a better way. I CANNOT fathom having to endure stent living for the rest of my life. You are amazing to march on despite the pain. It is not for the faint of heart. .
I have described the pain to everyone the same way, like barbed wire twisting through my insides. Pulling down on your organs, making you double over. The pain the Utterer stent causes a woman is no joke. I was working as a sales associate, crying in the bathroom, waddling around on the sales floor in pain when I should have been at home resting. My Doctor only warned me of some discomfort, that was such a lie and they know that! I will never allow another stent to be inserted into my body ever again, I would leave it up to God.
My body has been through 5 neck surgeries, one was traumatic. I’m currently waiting for a back surgery and have severe nerve pain.
but let me tell you, that nothing compares to the pain of a stent!
It should be a crime! It’s Barbaric!
Next time I get a stone, I’ll just pass it on my own. No thanks….
It’s not nearly as bad as I expected!
I had my ureter stent removed about an hour ago. It was in for 17 days due to a kidney stone surgery.
I read all the horror stories so I took 4 Advil and one pain pill about an hour ahead of time. Note! The urologist did not give me this advice, I did it on my own.
I was very nervous. If I had it to do over, a Valium would have been better to calm my nerves.
I literally closed my eyes and counted out loud to distract myself. The room was scarier than the procedure. It looked like an office sized operating room. The nurse cleaned my private parts, cold lidocaine added, noise of some machine which I think was saline solution pumped slowly into my bladder. The doctor came in, I kept my eyes covered, he spoke to the nurse, I counted out loud, said OW twice in the 45 seconds it took him to remove it and it was ove!.
Pain was maybe a 3 or 4 only for a second then it was over.
The worst part was the build up in my mind from reading horror stories. Honestly it didn’t really hurt. If I ever have to have this again, I’d request Valium, that’s it.
Now, I can totally feel that tube is gone. I can sit upright like at a desk or kitchen table without that pinching feeling from the tube. No blood in my urine but a little cramping. I unbuttoned my pants and the cramping went away.
Good luck. You Can do this! If you’re truly freaking out as the doc ahead of time for a Valium.
I used to respond to the shock wave lithotripsy, but that soon ended. Then I moved to the ureteroscope. Yep. Stent. What a hell that was. I was flat on my back for five days. I ended up in the ER on day 2. It was a week of vomiting and at the end, I was constipated like crazy. It was like giving birth again but from the rear.
More stones a year ago. I outright refused another scope. No way was I going back down that road. That meant a PCNL. I thought, “please. I can handle a small incision..but a stent? Not so much”. I’m here to tell you you do NOT want a PCNL I was one of the 10% that went home with a tube in my back for FIVE WEEKS. Every week, I had to go back to interventional radiology where they went back through the incision and poured in the contrast to see if the blockage cleared. If not, the partial stent (higher one and nothing like the one in the bladder) was put back in place and on my way I went. Did I mention it is NOT medicated? It did NOT feel good AT ALL.
Enter 6 months after that. Stones. Again. Now, 9 months after the PCNL, I’m in bed with a stent. Again. Shoot me.
When this bad boy comes out, I’m keeping a 2 liter bottle of water in the refrigerator at ALL times. I’ll go zero sodium, calcium, protein, and oxalate. Did I mention I’m also am supposed to be gluten-free and am supposed to watch my sugar, too?? LOLOL I’ll have to graze in the lawn, but I will NOT EVER go through this crap again.
Update: Second stent was not NEARLY as debilitating as the first. Oh, it gets jarred if you sit wrong and I pee’d razor blades for a day. I couldn’t be on my feet long because…gravity. HOWEVER, I’m not bedridden nor vomiting (did that once after the procedure). Maybe the damn ureter is stretched enough now with all the crap it’s had to go through?! Still not fun, but nothing I’d outright refuse no matter what (like the first experience). Now I’ve got to get the courage to yank it out myself…😩
I have had stents for several years and will the rest of my life. They are miserable, painful and at times feel like I have metal rods stuck in my body. There is always bleeding and infections with abundance. I have had them to fall out 12 times just last year and the pain be so bad that I thought my only relief was death. Then they are shoved back in without the benefit of anesthesia and pain meds only to fall out again in the next day or two and heading to emergency surgery. I weigh less then 100 pounds and the spasms are so bad that two nurses have to hold me down. My issues are damage from chemos and radiation. I can no longer jog, hike, ride horses etc. I am basically stuck at home with limited life. Last year alone, I had 32 infections and 7 surgeries. My urologist, whom I think it the best doctor ever and I have come up with a working tolerance. I don’t lift anything over 5 pounds. At 8 pounds I bleed a lot. Only drive 20-30 a day. Drink as close to a gallon of water as I can and take 6 cranberry pills. I have only had 3 surgeries this year and so far (Sept) only 6 infections. I know there is a need to them, but can’t there be something that makes them more tolerable? The metal rod or sword feeling is no fun. Trying to sleep or even sit in comfort is not easy to do. There have been a couple of times that they were not to bad at all, just a little discomfort. Sometimes you break out into a cold sweat and throw up from the pain raging.
Very informative. Two previous stent placements after surgery to remove large stones were not that problematic. This third, most recent stent is quite noticeable, causing a great deal of pain. Odd thing was that the pain did not begin until a few days after surgery & subsequent placement. Calls to the urologist’s office did not provide helpful information–other than to visit E.R.if a fever begins. Can’t tolerate most prescription pain meds so Tylenol & Advil are the only options. Would be great to find some temporary topical analgesic safe to apply externally. Got more info here than from the doctor’s nurse. Great blog!
My right kidney was shrinking is why I had to have a stent. I felt everything and will always have it. For some reason I can not talk above a whisper which hurts my throat when I try to talk. I know it cant be from the stent but its been 6 months and throat is no better I don’t have kidney stones.
If you had general anesthesia for the stent placement, tge voice problem could be related to the breathing tube. You should contact the anesthesiologist and maybe an ENT to get your larynx examined. I’m a postop RN and have only seen this once but could happen!
I am sorry for your condition. I had a kink in my urethra tube stopping the flow of urine to my bladder. I have had 2 different stents, 6 months apart. Both are horrible even though they did what they were designed to do. I will have a 3rd stent in March and forever six months apart.