We know that the prospect of needing to have a stent removed is a big source of anxiety for patients. While almost everyone can’t wait to have his or her stent out, not knowing what to expect during the removal procedure can be just as bad. To better prepare you for your procedure and perhaps relieve some of your concerns, we asked visitors to the website who have already gone through the process to share their experiences with you. The results of our stent removal survey follows. Thanks to everyone who replied and let us know what you think in the comments below.
 How are people having their stents removed?
How are people having their stents removed?
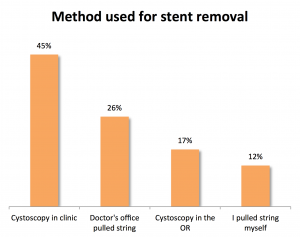
575 of you have responded to the survey over the last 3 months that it has been up. The most common method of stent removal was through the use of a flexible camera placed in the urethra (cystoscopy) in the doctor’s office, with almost half of respondents reporting this approach (45%). 17% instead had their stents removed using cystoscopy in the operating room. 12% removed their stents themselves by pulling on a stent string while the last remaining 26% had their stents removed by having their doctor’s office pull on the string. Our post on stent removal describes these techniques in more detail.
How much pain should I expect?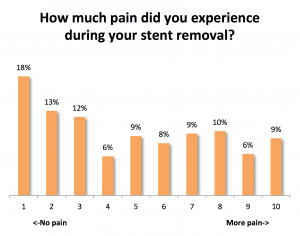
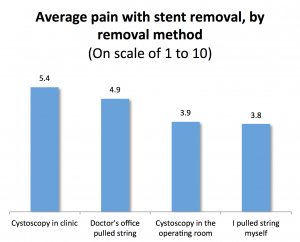 Out of a scale of 1 to 10, with 10 being the worst pain ever and 1 being no pain at all, the overall average amount of pain reported was 4.8 or a moderate amount of discomfort. However, it may surprise you to hear that the most common rating given was 1, or no pain at all, chosen by 18%. So while some patients do report a high amount of pain with their stent removal, many had no pain or only mild pain. If we look at pain by method of stent removal, average pain was relatively higher for those who had their stent removed by office cystoscopy (5.4 out of a scale of 1 to 10) followed by doctor’s office string removal (4.9), operating room cystoscopy (3.9), and self string removal which had the lowest reported amount of pain (3.8). However, these differences between method of removal are not dramatic given that the scale goes from 1 to 10.
Out of a scale of 1 to 10, with 10 being the worst pain ever and 1 being no pain at all, the overall average amount of pain reported was 4.8 or a moderate amount of discomfort. However, it may surprise you to hear that the most common rating given was 1, or no pain at all, chosen by 18%. So while some patients do report a high amount of pain with their stent removal, many had no pain or only mild pain. If we look at pain by method of stent removal, average pain was relatively higher for those who had their stent removed by office cystoscopy (5.4 out of a scale of 1 to 10) followed by doctor’s office string removal (4.9), operating room cystoscopy (3.9), and self string removal which had the lowest reported amount of pain (3.8). However, these differences between method of removal are not dramatic given that the scale goes from 1 to 10.
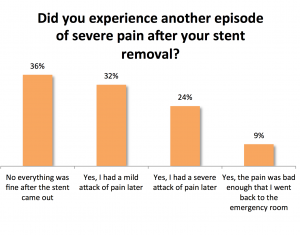
Will I experience pain afterwards?
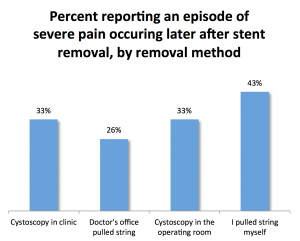 Most patients had no pain or only mild pain after their stent removal. Unfortunately, a third of patients (33%) did experience a severe attack of pain after their stent removal, including an unfortunate 9% who required a return trip to the emergency room for their pain. When comparing recurrent pain by method of stent removal, severe pain occurring after stent removal was more common in the self string removal group (43%) and less likely in the doctor’s office string removal group, office cystoscopy, and operating room cystoscopy groups (26%, 33%, and 33%, respectively). It’s not clear why those who pulled out their own stents were more likely to report a severe episode of pain afterwards. There is some evidence that taking a tablet of an NSAID medication (naproxen) before removing your stent can help reduce the chance of experiencing a severe episode of pain.
Most patients had no pain or only mild pain after their stent removal. Unfortunately, a third of patients (33%) did experience a severe attack of pain after their stent removal, including an unfortunate 9% who required a return trip to the emergency room for their pain. When comparing recurrent pain by method of stent removal, severe pain occurring after stent removal was more common in the self string removal group (43%) and less likely in the doctor’s office string removal group, office cystoscopy, and operating room cystoscopy groups (26%, 33%, and 33%, respectively). It’s not clear why those who pulled out their own stents were more likely to report a severe episode of pain afterwards. There is some evidence that taking a tablet of an NSAID medication (naproxen) before removing your stent can help reduce the chance of experiencing a severe episode of pain.
How did the experience compare to what you expected?
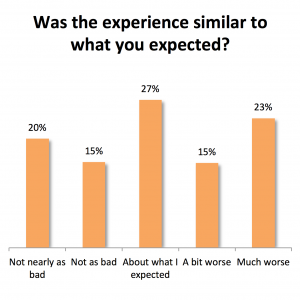
Overall, 35% felt the actual stent removal experience was not as bad or not nearly as bad as they expected. 27% reported that their experience was about what they expected. 15% felt it was a bit worse and 23% felt it was a much worse. Reporting the pain as much worse than expected occurred in 27% of those who underwent office cystoscopy, 24% of those who had their stents pulled out by the clinic, 20% of those who pulled out the stent themselves, and 15% of those who had a cystoscopy in the operating room.
If you had a choice, would you choose this option again?
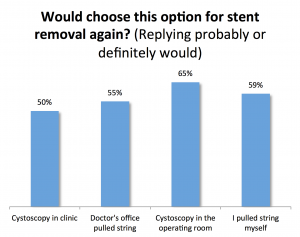
Those who underwent operating room cystoscopy to remove their stents were most likely to choose the same technique again (65% replying probably or definitely would choose this method again) followed by self string removal (59%), doctor’s office string removal (55%), and office cystoscopy (50%).
While we asked respondents whether they would choose the same method for stent removal the next time, not all options for stent removal may always be available to you. For example, your doctor may choose not to use a string if he or she feels that your stent needs to remain in longer than a few days because the string can easily get snagged and the stent might accidentally be removed too early. Secondly, stent removal in the operating room is not always an option because: time in the operating room may not be available, the risk to you of undergoing anesthesia again may outweigh the benefit of having the procedure done in this fashion, the costs to you in terms of time and money involved in scheduling and preparing for an operating room procedure may not be worth it. We recommend that you talk to your doctor to go over the best option for stent removal in your particular case.
Priorities as a patient:
We asked respondents how much of a priority certain things were to them as a patient with a stent. Being informed why a stent was placed was the biggest priority for respondents (4.7 on an importance scale of 1-5). Being informed about what was actually involved in the stent removal procedure was also a high priority (4.5). Being able to have general anesthesia was a moderate priority (3.1) while being able to see a video/diagram of the process was a lower priority (2.9).
Okay, what’s the bottom line?
Most patients reported an average amount of discomfort with stent removal by any technique. Many patients actually reported no or minimal pain but about a third reported significant pain. Removal by office cystoscopy was associated with more pain on average and removing a stent yourself by pulling on the stent string was associated with less pain on average. A third of patients may experience a delayed attack of severe pain after their stent removal. Overall, about 62% reported that the experience was not as bad or about what they expected but 38% said it was a bit worse or much worse than they expected.
Editors note: Post updated on August 29th with additional survey results.
My stent removal was done on 3-10-23 at mid morning….,I was fine minutes after the stent removal at the PA-C office and she told me that I could get an episode of spasm or few after the procedure but it was rare…. Really ?? I got it after an hour when we were at Home Depot since “I was doing good” and in minutes I barely could jump back in the car for my husband to take me home to my bed and taking 2 Advils. I was feeling that my left flank was about to explote..was very painful from 1-10 scale..I created the 11 option. I spent the rest of the day at bed with painkillers and a bit of nausea. Husband talked about ER, no way ..was no going to happen.
Today is 12th and still I am in pain but much better of course, time to time I feel like electric shots in the lower back but less duration, this left flank still giving me hard time and I am drinking plenty of liquids ..
To sleep … I have some problems lying on my side (on either side) I feel pressure on the left and my flank hurts and on the right I feel that the organs lie on that side and it hurts too… until finally I sleep for a while because I have to go to the bathroom…
I hope and pray for this situation to go away soon ..I was battling with a kidney stone since 12-26-22! Is too much for me ..
Not happy going in again second time for kidney stone removal surgery to remove a 2 mm stone that doesn’t want to pass. Doctor is going to put in a stent again and I hate it the pain and reminds of the last time. Plus when he removed my last stent no numbing, nothing, hurt so dam bad
I’m frustrated because I feel like you are doing surgery to remove the Stones get them out………
Tired of dealing with them it’s definitely not fun.
I recently had an 8mm kidney stone stuck in my ureter. My doc recommended we go get it. I went in, was put under and woke up needing to pee and noticed a string hanging out. Lovely.
My doc told me in 10 days I could pull the stent out myself. I thought he was joking. It wasn’t funny. But he was indeed serious. For the first few days, the opening of the urethra burned a bit. I assume this is because my doctor drove a Buick up my urethra. AZO and a few Tylenol helped a great deal. By day 3 the urethral pain had mostly subsided.
For the next 10 days I was keenly aware of my stent and dangling string. I had no shortage of those wanting to drag me around by it or pull start me. However, behind my laughter, I was terrified. For the next ten days, I was committed to taking it easy and not letting that stupid string run away inside of me. While I was unsure of what removing the stent at home would be like, I knew if I lost that stupid little string, my doc would be pulling into the room in that Buick again – a far worse outcome.
Unlike women, let’s just say guys have a variable urethral length. I was keenly aware of such variation. If I noticed anything whatsoever changing at night, I jumped out out bed, shut Mr. Happy in a door and immediately turned on Ernest Borgnine on McCale’s Navy or Gunsmoke! Borgnine is now my hero. I was not going to lose that string!
Overall, when I urinated, I felt slight discomfort in my right kidney from urine traveling up the stent – but it was nothing I can call pain – a dull ache at most. Take it easy and take a Tylenol. Drink lots of water. The discomfort in my case was nowhere near what I expected. Mild at most. I didn’t feel the stent but wanted to pee far more often than normal. I noticed this most at night.
On day nine my anxiety was in full bloom. I had read every stent removal horror story on tne Interwebs. I made a will and notified my next if kin and answered their questions about any inheritance that might receive. Quite the want-list they have! I also learned that no matter how blessed you are as a man, you’re nothing more than a sniveling gerbil when confronted with the removal of a ureteral stent. It’s natural design.
Day 10 arrived. I took 2 Tylenol and an Aleve. I returned from shopping and thought I’d do a string check. Yea! There it was. I thought I’d pre-tug a bit of string to see what I was in store for. I stood over a towel aimed about 45-degrees downward and gently pulled on the string. There was mild resistance but the string was coming out. I pulled it an inch at a time waiting for the crushing pain I’d heard about. After about 10″ of string I found myself at a point of no return. I continued gently – teeth clinched. The plastic appeared. I continued. 1″ at a time. The plastic finally emerged – curls and all.
The truth was that my stent removal was overall a non-event. Other than a few tiny drops of blood at the very beginning nothing adverse happened. I had no sensation inside of me of the stent passing through me. By doing it myself, I was able to position the angle of the string in a way that was lined up with my urethra. I adjusted a few times when I felt minor discomfort. It worked. Your doc or a nurse doesn’t know that. I am certain that causes a great deal of pain for most. I peed immediately and noted a few tiny clots. No pain.
For most, I suspect the anticipation of the unknown is the scariest part. The great news is that most people I have spoken to report similar experiences to mine. The ones who had it rough, said the worst part was the removal of the stent by a doctor or a nurse. As it turns out, home removal is likely a better solution if you can endure the expectation of a horrendous death!
Hopefully my experience can help you understand that it really isn’t anything you cannot handle. In my case, it was so much less than I wanted to believe.
Thank you for sharing your detailed and humor filled experience. I felt A LOT better after reading it.
This resonated with my experience as well, minus having a penis. That said, three days later and I’m in so much pain, and I’m peeing out blood clots, but the actual removal was painless.
Well your story helped me a great deal. I just removed the stent that had been placed in me after my stone surg. The only thing I could add is that doing this in the shower worked well for me. Also I had a great sound track going on my phone. The best was Willie Nelson’s music. Pretty much just take it slow. Thx
Hilarious! Love it, and thanks for the encouraging words. Read it to me wife and she was shedding tears of laughter. I think taking pain killers before removal is extremely helpful.
Just had Stent removed about 3 hours ago, in Doctors office. A CAT scan showed kidney stones, so a Stent was recommended. Blasting of stones of chalk considency, resulted on needing to keep the Stent for 4 weeks, just to make sure stones were gone. No issues with having Stent. Did as I was instructed by Doctor.
Removal was simple & done in office.
Mild pain, mild pressure & little or no discomfort. (I have a hi tolerance for pain) but the anxiety of the unknown can peak stress & discomfort, so relax, do as your told, and take it easy. I’ve had a hysterectomy & know that if you take care of yourself you will come thru just fine. Yes, there are exceptions but doctor is always just a phone call away.
Now to relax, take it easy & lay low for the rest of the day & night!