What is a stent?
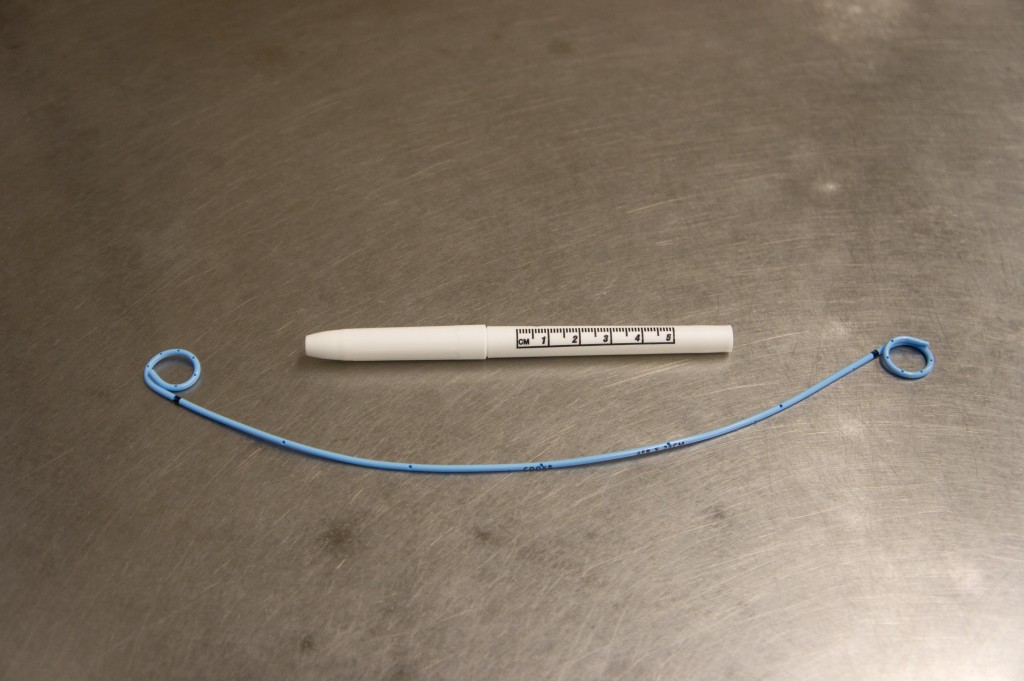
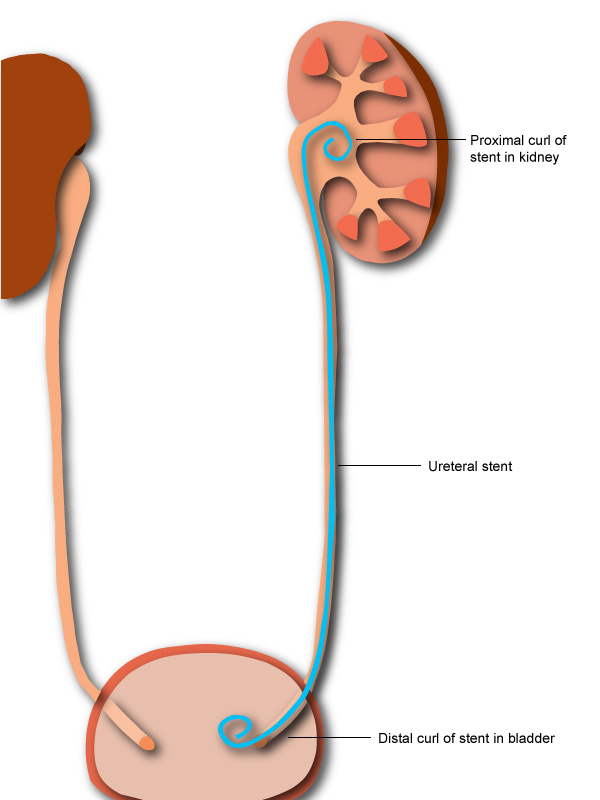
Ureteral stents are soft, hollow, plastic tubes placed temporarily into the ureter to allow drainage around a stone or to speed healing after a stone surgery
When are they needed?
Stents are used for various reasons in patients with kidney stones. They may be placed in patients to help reduce pain from a stone, when infection is present to allow drainage, or when a stone is preventing a kidney from working adequately. Stents are also commonly placed after surgeries for stones, as in ureteroscopy, to allow healing and prevent swelling of the ureter.
How is a stent placed?
Stents are placed during surgery by sliding them over a soft “guidewire” which is placed up the ureter, which is the tube draining the kidney. See a video below of a stent being placed.
How is a stent removed?
Stents can be removed in two different ways. Sometimes, a string is left attached to the end of the stent. This string is allowed to come out of the patient’s urethra, the tube where he or she urinates. The string can be used to pull on the stent and remove it. In cases where a string is not left attached, a small camera called a cystoscope is inserted into the patient’s urethra after numbing medication has usually been administered. The cystoscope is then advanced into the bladder and the stent is grasped with an instrument and removed. See our post on stent removal for a video and more details.
How long can a stent stay in?
In general, most stents should only remain in for no longer than 3 or so months. If a stent is left in too long, it can form stones directly on it, making removal difficult.
What are the symptoms of having a stent?
While some patients with stents have minimal discomfort related to them, other patients will report symptoms that can range from being annoying to being severe enough that the stent has to be removed. These symptoms can include:
- Sensation of needing to urinate
- Seeing blood in the urine
- Bladder spasms
- Burning sensation during urination
- Pain in the back during urination or when moving
- Pain in the bladder
Is there anything that can help reduce the discomfort of a stent?
Different medications may be given to help reduce the discomfort of a stent. The most effective appears to be those from the alpha blocker class of medications including tamsulosin (Flomax) and Alfuzosin (Uroxatral). Other types of medications commonly given for stent discomfort, such as oxybutynin (Ditropan) or phenazopyridine (Pyridium), do not appear to be successful at reducing stent related discomfort in placebo controlled studies. Traditional pain medications are also less successful at reducing stent discomfort.
Hasn’t anyone come up with a better stent?
Research into improving stent designs will hopefully reduce the discomfort associated with them. Innovative stent designs currently being tested include stents embedded with medications to reduce discomfort and stents that dissolve by themselves.
I’ve had chronic kidney stones for 33 years. They started with both my pregnancies then remained fairly quiet until I turned 40. They came back with a vengeance now. I’ve had numerous laser lithotripsy treatments and in 2021 I had to have a percutaneous nephrolithotomy(surgery where they go through your back to remove the stone) as I had a 2cm stone and that’s too big for lithotripsy. I just had another lithotripsy 5 days ago as I have some more whoppers in there around 1.5cms. Well the doc tried to get into my right kidney but the path was obstructed by a stricture(narrowing) in my right ureter that would not allow the scope to pass. He inserted a stent that has to stay in there for a month and then he’ll try to go in again to blast the stones.
I am beyond uncomfortable and I’m so bloated I look 5 months pregnant! I have a burning pain in my right kidney and sharp pains all the way down to my urethra. I feel like I have to pee all the time and moving around irritates the shit out of it. Any Dr who says you’ll have some minor discomfort with a stent is a bloody liar. I think all urologists should have to have a stent for a month.
Hang in there everyone. (Btw,I’m a retired RN so have some medical knowledge about all this. That sometimes makes it worse)
Bloody spot on Adrienne! I’ve had more stents than hot dinners and they do not get better at all. It should be a requirement for any budding urologist to have one of those bastards shoved up their bits and left to go about their day to day lives. It might give them some perspective about the pain and discomfort.
I’ve explained to my various urologists over the years that the stent experience is not ideal. I’m a fairly direct guy and have told them that, “can you imagine pissing a prawn out backwards while you’ve got a clamp around your kidney and bladder? Well that’s nothing compared to this fucking stent.”
As per my last stent experience (as written below), the doctor sidled up to my bed and told me that he was going to pull the stent out; it was the string one.
Let’s say that he pulled it with so much gusto, I’m surprised that my cock didn’t rebound off my belly and slap me in my face. It took every fibre of my sanity and good natured disposition to not headbutt him in pure white hot, pain fuelled rage. And the absolute audacity of him to seem surprised and then say, Cmon, it’s not that bad.” Don’t get me wrong, he is a lovely bloke but I feel that Karma needs to play out in a similar way for him one day.
Anyhow, there is a good chance that I will become ranty if I continue on the way I am.
To those of us out there suffering from or ever having experienced the devil’s diamonds, stay as well as you can. In Australia we have a saying that essentially highlights when something particularly adverse has occurred… “C#%t’s fucked!” I feel that stones and stents meet the correct criteria for the use of this phrase.
I could have written that myself. My situation exactly.
I ended up in ER because my stent was blocked. My bladder emptied with a catheter 1.4 liters. I am absolutely miserable. Are there any other options?
So, from what comments I have read everyone is saying they are removing stents at home. Is there anyone that isn’t?
I had a stone surgically removed on Monday morning, stent put in, and it’s to stay 1-2 weeks (awaiting confirmation for appt). I go back into urologist to have it removed when it’s time, and I was given an antibiotic (2 pills) that I take the day of stent removal (one that morning and one 12 hours later). Just curious if it’ll be painful or how that works.
Right now, I have minor discomfort in left side (not as bad as it was prior to surgery and sharp) and a lot of bladder issues (spasms, running to pee every 10 min, and major sensitivity).
I had an emergency stone removal on my left side in May 2023, had a stent with a string to remove myself. It was awful and not “just like removing a tampon” that the nurses insisted on. I had full stone removal from both kidney’s last week and have two stents and have appt for urologist to remove next week. I too have minor discomfort and constantly feeling the need to pee – much more so then last time. At this moment, prefer the stents that I do not have to remove myself.
I’ve had both. I liked the one you take out yourself. I had one taken out this morning, but it had to be done at the drs with a scope. Not fun, and have some pain afterwards. No string on it. When they say they are going to numb the ureter, you know somethings coming.
so just had two stents put in two weeks ago they lasered 13 stones from 5mm to 14mm had the soft stents with strings yea two days then im to remove them at home that was a experience i dont wish on anyone then all the stones coming out now im dealing with the burning from what i guess is a uti im taking pyrdium and flowmax no more pain meds but im good pain wise just alot of urinary discomfort and it feels like i have to go all the time i have to keep track of my bathroom and water intake anybody have this problem
I had a 12mm stone. My Urologist used lithotripsy and shockwave to break it up and put a stent in after. I was to pull it out in 5 days. When I arrived home I was uncomfortable. After a couple of hours and lots of bathroom visits I noticed that my stent was sticking out! I called a friend who is a nurse and she had me call the on call number because it was after hours. (Of course it was.) They told me to just go ahead and pull it out. Reading some of these comments I am really glad it came out. I had enough pain and misery waiting for the debris to empty out to last me a lifetime.
My wife had a ureter stent put in in April of 2023, she had an extremely high amount of ecoli present in her urine and had a 3mm kidney stone present causing internal lacerations which they feared would become infected and cause sepsis. The urologist put the stent in to help drain her bladder and allow the ecoli to be treated safely. The problem is now that they want somewhere around 16k to remove it. She is literally mentioning suicide everyday now because she can’t bear the pain. We don’t have insurance, and I even lost my ability to work because I had a STEMI in October of 2023. I am a veteran, so I had free healthcare. She is not and not even a public healthcare system can help because it is overcrowded. I’m literally at my wits end and do not want to lose my wife. This thing has been inside her for almost a year now, she’s incontinent now, cries all the time, how do I get this thing out of her? It does not have a string attached. What is a local anesthetic OTC I could use to numb the area and any ideas how I could possibly extract the stent safely?
Go to the E.R. as a last resort. They cannot deny your wife, especially if it’s life threatening like sepsis.
I hope she got this resolved. I don’t see why that costs so much, they remove it at the drs office. Leaving the Stent in too long can cause other issues. Hope it goes well for her.
This Stent Journey has been a whopper! Reading all your comments here has been so helpful…we are a unique Community indeed!
Nothing has been easy or painless so far… But the 9mm stone is at last lasered and gone.. Yay!
Sent home with the charming Stent with a String model…More pain…1 week and I can pull it out at home…
Concerned about what that is going to be like!
Anyone have good insight/advice on removing the stent at home?
Great Dr. but not much help about what to expect on this next step…
Would love to get my life back!
Thanks!
I think it’s too late to reply now but I was thinking of a way to describe it. I had my stent with a string removed at the urologist office. Are you the type who rips off a bandage or slowly remove it? My urologist ripped my stent out quickly. It felt as if she was ripping off duct tape from my most sensitive area. I hope to never have to go through that again!
I had 2 stents put in – one in each side after surgery. I think that the movement of them inside or something caused enough irritation that I ended up going to the ER. They asked for a urine sample and it was so bad it just came out pure blood. They gave me some pain meds. And then when it was almost time to have them removed, I just ended up pulling them out.
Maybe they were too long or something? I have an upcoming surgery and he said that they go by your height, but maybe something about that equation doesn’t add up.
I also asked the nurse about how many days that I would have afterwards before I went back to work after the uretorscopy and she said none. And it’s like how am I supposed to be revved up and rearing to go back to work the next day? If it keeps going like this – they’ll have us working as they are doing the surgery.
I had my stent put in yesterday and I think I will have to ask them to remove it today. This was supposed to fix my back pain, not make it worse. My reason for a stent is different from others here. I recently went through endometrial cancer (last year), had a complete hysterectomy, and thought I was in the all-clear. Had a clear PET scan 3 months ago. But I was experiencing terrible pain last week so I went to the ER. When they did a cat scan they discovered a new mass pressing on my ureter. So they recommended a stent in the ureter to ease the back pain. Supposed to get a biopsy on the mass but it is not scheduled yet. Well, this stent is awful. It feels like a sharp stick is in my urethra. ( kind of like a Tampax put in wrong- painful to walk and certain ways to sit. Laying down only makes it worse) I am going to tell my male doctor it would feel like a stick was in his penis. See how that would feel. I thought once it was in place, I would not actually feel the stent. I expected pain and discomfort when peeing, but not this. And he put a longer-term type stent in because he said it may take a while to figure out this whole mass thing. If it is cancer (and even if it is not), it’s got to be removed. Anyway, sorry to rant, but I’ve got to get this damn thing either out or fixed. This can’t be right poking against my urethra, can it? I was better off with the back pain.
Wow. Just unbelievable what medical professionals are doing and the cameras that can capture all these fun things in which I partake
I’ve left a couple of posts over the years describing the trials and tribulations of being host to a stent. Oh boy, this time was, by far, the absolute worst experience of my kidney stoner life.
As I’ve posted before, I’m your everyday Aussie bloke (now 41), I have a couple of kiddies and a bloody wonderful wife. I live in a small country town and I work in the emergency services sector.
Tuesday night, I start my shift at 6pm. It’s bloody cold outside and I’ve decided to work as an Alpha unit; to get some of my own damn work done for once.
About 8.30pm, I’ve just finished being yelled at by someone, politely finish the conversation and walk to my vehicle.
Hmmmmm….. why is my side sore? The appendix is on the right side. Perhaps I had gone a tad too hard with a few wines and beers over the weekend. Nah, she’ll be right. I’ll just shake this shit off and continue going about my very important business.
9.00pm. Fuck. Fuckitty, Fuck McFuck…. Apologies for the language (I’m sure you’ve all used it in these particular situations yourselves), my right side is pounding like Thor in a brothel. His mighty hammer smiting my insides with enough force to exorcise all my lifelong sins. This isn’t good but I have work to do.
9.45pm. I feel the pressure in my kidney build. It was like one of those dudes that services the NASCARs when they pull into the pit stop; changing and inflating the tyres… you know, quickly and without delay. Take ‘em off and put ‘em on again, thanks for coming.
Yep. The pit crew decided to set up in my right kidney and left the air compressor on.
10.00pm. Panic sets in. Jobs are piling up, I’ve got so much pressure in my guts, if I use the shitter I’m likely to demolish half the building. I’m sweating, my heart is beating faster than the time I had a wank in a sauna and I’m feeling faint. Keep it together little fella. You can get through this.
10.15pm. I feel that lovely hydronephrosis start to kick in. That feeling that your kidney has turned into a football. This is not good, not good at all.
I sheepishly wander over to my supervisor and say, “hey big fella. I’m fucked. I reckon my kidney’s blocked off. I might have to finish early.” My supervisor shrugged and asked if I wanted a lift to hospital. I politely declined. I didn’t think it would be appropriate to be making grunting noises whilst in the presence of my workmates. Of course in the situation where car keys are exchanged and wives are there, well that’s different 😉🤣
10.30pm arrive at ED. The lovely nurses look at me and say, “Oh AJ, back for the same again are we?” I nodded and told them that I thought my kidney had blocked. There were a couple of worried glances and a phone call was made to get the radiographer out of bed and come and CT scan the shit outta me.
11.00pm. 150micrograms of IV fentanyl hadn’t touched the sides. I was in a state like no other time before. More worried glances and a nurse is placed next to me for monitoring.
11.30pm. Radiographer arrives. “Hi AJ, same again is it?” I nod my head and tell her it feels much worse. I’m dosed up on more pain meds so I can lay down and am run through the radioactive donut.
Moments later I hear an, “Oh dear. AJ was it your right side that hurt?” I nod in the affirmative. I’m told that there is a blockage and I’ll have to got to the nearest town for surgery. Yay! What a fucking fantastic night.
Wednesday morning 9.30am. Transported via ambulance to big town hospital. En-route, I felt every bump and lump in the road to the point I sat up and started doing Stevie Wonder facial expressions. Paramedics see that I’m in a spot of bother and administer some ketamine.
That was quite the experience. All I can say is that I ended up telling the paramedics that I couldn’t breathe and that I was scared of the trees outside. I realised that it had worn off when I found myself hugging the female paramedic and rocking like I’ve never rocked before. I may have even been stroking her hair and telling her everything was ok.
11.00am. Arrive in big town hospital. Wheeled into ED there and left to my own devices until a surgeon comes to see me. Yes, we have to unblock you, stent you, blah blah fuckity blah. Yeah I know. I’ve done this once or twice before. I spend the remainder of the day in ED and am transferred to the surgical ward later in the evening.
Thursday morning. I wake up in so much pain and pretty much scream the place down. A rapid response team comes to my rescue and places a spinal catheter in me, dose me with ketamine and performs a spinal block to stop the pain.
Later in the morning I am wheeled into surgery for stone removal and stent placement.
About 3pm, I wake up in all sorts of pain. I am wide awake and in agony. At this time I was told the stone had perforated the ureter wall and leaking urine was aggravating my insides. No shit Sherlock! Aggravating my insides? Try having a fucking barbecue on my balls, bladder, kidney…. Nah fuck it, it would just be easier putting me in an oven with an Apple in my mouth and some herbs up my arse.
Anyhow, I could go on for ever with this nonsense but I shan’t.
I am currently laying in hospital, just having had the stent removed and writing this for your voyeuristic pleasures. Just to add smoke to the wind, my surgeon tells me that I really should have had the stent in for 6 weeks for the perforation to heal. I’m likely to get another stent if anything happens in the next few days. Oh, and for you cheeky nuggets that like to compare sizes, mine was 5mm. I’ve passed bigger before but this is the one that shredded me.
Right now, I’m happy the stent is out. Stents and perforations are not fun, I can promise you that.
First of all, you missed your true calling … “ a writer” 😅
Sorry you had to experience all that!! I had 6 stones lasered and a stent
Inserted for 6 days and took out myself. An hour later all he’ll too broke out, the cramping
was worse then the stones . Getting stronger every day. ..
Stay well !
I’m researching stents and came across your story, which is funny, yet scary as hell! I, too, have had many stones, latest have passed two 6mm with little problem. Skip to now, I have an 11mm setting up residence, which was 8mm 3 months ago. Needless to say, lithotripsy is to be Monday morning with stent placement. I’m more than nervous about it, had one stent previously with little problem, but the removal was a b*tch! Just want to say your story cracked me up and gave me a little humor. Hoping you have had no further problems since then. Thank you! 😊
So my first lithotripsy was Fri, Oct 13, and woke up with no stent, hurray! No problems whatsoever until the 2 week follow up X-ray which showed the whole 11 mm stone was still there! The lithotripsy didn’t work 😱. At all! 5 to 7% chance of that! So had a laser surgery with stent placement. This stent is the most uncomfortable thing I’ve ever had, not counting the blood in urine. I never passed any fragments and blood finally stopped a week later, but this stent has to go!! My appointment is in 4 days, if I can stand it that long! I feel for anyone that has this nightmare thrust upon them. There has to be a better way! Hoping my story ends with the removal of this stent!
Stents are the most painful devices perpetrated upon me and I have had 2 children, frozen shoulder and a broken pelvis. It is difficult to believe that out of the thousands of urologists around the world this is the best they can come up with. Perhaps if they were all forced to wear them for a week or more incentive would help them be more empathetic and creative.
I totally agree. The pain has been excruciating. The doctors just don’t get it!
Hello everyone. I have two kidney stones Atleast – one is too big to pass. I believe 6mm. I have had a stent put in and whilst the pain is not as intense as the stones was I’m finding it really uncomfortable. Increasingly painful, I relate to the “tampon falling out” posts. I’m also 32 weeks pregnant so I have no other option but the stent, they said baby is pressing on it as well so makes it worse. My removal is scheduled for august/September. I can’t have a lot of the pain killers recommended as I am pregnant – no anti spasm stuff or anti inflammatory. I’m considering acupuncture. Anyone got any tips for what I can do to ease it or help whilst pregnant?
Try Reiki sessions. I’ve had a stent for 4 days now, and was experiencing much pain and blood in urine. I arranged a “remote” Reiki session, with a Reiki Practitioner, for yesterday morning. At the arranged time, I made myself as comfortable as possible, in a meditative, receptive frame of mind, and was amazed I actually felt her energy directed at my then-painful lower abdomen. The session lasted about half hour (I’d been in bed before that). The pain subsided without drugs, and lasted all day. Now, the pain is relieved,
For the Reiki session itself, my then-intention was just for the severe lower abdominal pain, as my Urologist had explained “…a little bleeding was normal…”, so I hadn’t been worried with the bleeding.
Please, remember that Reiki, as I was taught, works best with a specific intention in mind. Though it can be done for overall health, my intention at that session was just for the pain.
BTW, in the lineage I was taught, (due to factors beyond this entry), self-applied Reiki is less effective.
Since you’re expecting and it does preclude most drug-based interventions, (their “new-agey”-related associations notwithstanding), I highly recommend you consider Reiki. And Accupuncture is also an excellent alternative.
Wishing you the best outcome possible, for your renal issues, and your pregnancy.
Uggg having a kidney stent put in is the worse!!!!I feel like I’m being tortured…I really don’t know how much more I can take of this..I feel like I’m being stabbed and elecuted..I can’t function I understand they put it in to save the kidney but damn it’s been 6 weeks and waiting on date for removal of stones..nothing they give me helps with the pain…I’m totally miserable!!!!!!!
should have my kidney removal this time last year, it didn’t happen , I have had stent in four 3months awaiting my 3rd operation . Having a stent is the worst thing ever my life is on hold always feeling need to go to the toilet then a burning sensation when you move just restricted on what you can do, Dr said carry on as usual she needs to try having a stent
Melissa I feel your pain knowing what you are going through.
Hi, I had a stent placed on my right side ureter due to a 1cm impacted stone. The stone was not apparent during the procedure due to swelling. The Dr prescribed me with 500mg of Tylenol, 5mg of Oxybutynin, 200mg of phenazopyrid, 0.4mg of Tamsulosin. I’m 61 years old male, from a small country town in Tennessee with no ER I had to travel to 2 neighboring cities with ERs with no urologist that can’t perform any procedures of that extent. So I traveled to Nashville to a urologist there whom preformed the procedure but is very difficult to reach due to her busy schedule. I still have no idea what she planning on doing. Do you have any idea? I also have foam when I urinate into the toilet, is there a reason why?
The second she took on as a patient she became obligated to see you on an ongoing patient basis. In other words she cannot be too busy. Call the American Medical Association. Call the Tennessee Medical Association. If for Example you went to St. Thomas Ascention call the office manager. You have recourse. At your age it could be more serious than stones. Don’t take no as a reason.
How are stents removed when the procedure required a stint be placed in both sided.
I have one string. 🤦♂️ Not sure I want to hear the answer.
I’ve removed several from one kidney with little to know pain. My doctor just told my wife I can remove at home in 4 days.
I just pulled mine out. They were both encrusted and stuff.
Can a stent hurts both Kidneys, even though it is just placed on one side. I feel pressure on both sides, but my stent is on the right , Please help
This is what I’m thinking and I am by far not an expert. Just speaking from experience. Is it possible you have a stone on the left? It also may be referred pain.
I’m feeling the same thing. I’m in the er right now.
Stint is on the right and the pain is in the left. I need help too
I have passed hundreds of kidney stones since 1985. Have had lithotripsy several times and never had a stent and was just fine afterwards. That changed today.
I have passed stones as big as 8mm & 9mm without going to the er. From 2015 to 2019 I walked rough steep hilly trails 4 or 5 times a week. Passed 3 or 4 stones every month but never any bigger than 5mm and no surgery or er needed. My urologist said the hill climbing & running probably shook them loose before they could get big.
I quit walking the steep trails after plantar fasciitis got unbearable in 2019. Didn’t pass another stone until last year. I get ct scans every 4 months due to a 5cm cyst on my left kidney that hurts every day. I had a CT scan a few months ago that showed 18 stones in my kidneys. Biggest is in my right kidney 7mm a few 5mm and on down. The left kidney had the same amount of stones but 3mm ones and smaller.
The urologist decided he needed to take them out even though I can pass stones that size due to passing so many over the years. He was going to do both kidneys but decided to do the left kidney since I have pain there every day. My left kidney also has moderate renal cortical thinning so kidney damage. My right kidney never hurts.
So he decided to do a utereroscopy and leave a stent. I’ve never had a stent but my son has had 2 at once and was miserable. Dr said he would put one in so my kidney wouldn’t get blocked from the scope leaving the ureter inflamed or it would be like a stone blocking the flow. I passed a 4mm last week a few hours after my pre op appointment & i don’t even remember it coming down just felt some cutting down there for the last month sometimes that felt like a stone was about to come out.
The procedure today went fine until a few hours after i got home. I couldn’t pee for several hours despite taking Flomax, Piridium and another med he prescribed. So this built up the pressure in my Kidney that was like having a kidney stone blocking the whole time. With a kidney stone I can jump around, lay with my legs and back up against the wall and use all kinds of other tricks to make them move so i can empty my kidney. Today there was nothing I could do since there was no stone.
I was just about to call an ambulance when I finally peed. The cutting feeling from the stent hasn’t really bothered me but that pressure in the kidney was hell. I’ve peed alot since then and there’s still some pressure and a little blood left, Urine is orange from the Piridium.
Gonna try to go to sleep in a few minutes but I dread how it’s gonna feel when I wake up. I’ve used the heating pad and that does help. I’m lucky I only have to have this in for 3 days then I can pull it out. I can withstand a lot of pain but today was the worst I’ve ever felt. Nobody is putting a stent in me again!
My experience is very close to yours. At least 25 trips to the emergency room over the past 25 years.
Same thing has happened to me Tom
Same with me, I will never let them put a stint in me again. I could never pass a 12mm stone ever.
Have a stent still in my kidney after bladder surgery to remove cancer mass in bladder. Back pain was excruciating for a couple of days after the catheter was removed, but still have a 2/10 back pain when urinating and feel like having to go all the time.
Any recommendations on what to do before hand when the stent is removed, to avoid the pain of that process? heating pad on back before? start taking hydrocodone a couple hours before? or just put a stick in my mouth to bite on during the procedure?